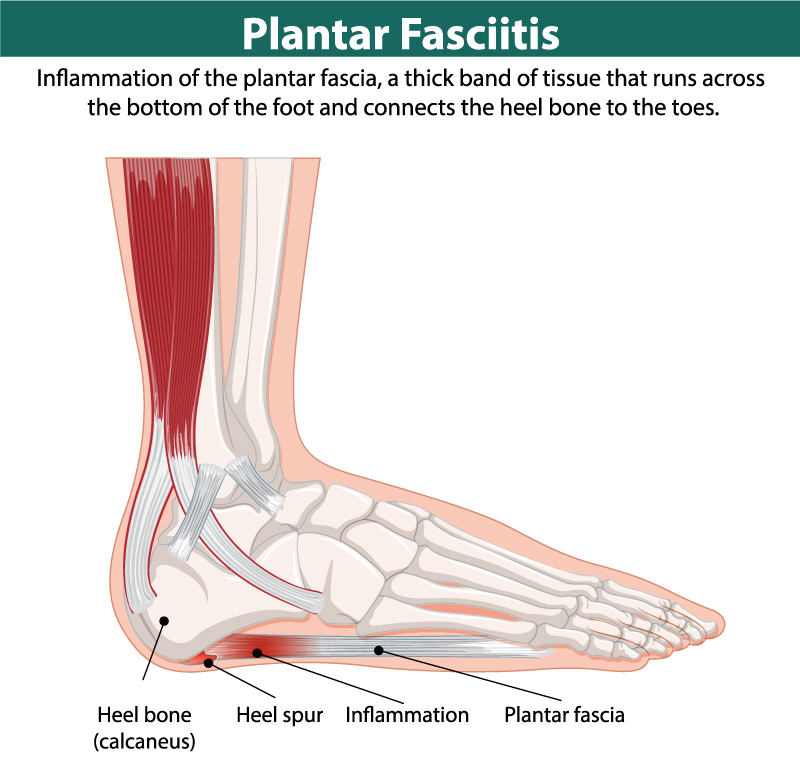
If your first steps in the morning bring a stabbing pain in the heel, or if your foot aches after a run and stiffens when you sit, you may be dealing with plantar fasciitis. The plantar fascia is a thick, spring-like band of tissue that runs from your heel bone to your toes, supporting the arch and helping absorb shock. With every stride, it lengthens and recoils like an elastic strap.
When training ramps up too quickly, shoes lose their support, or calves and ankles are tight and weak, this tissue is pushed past its limit. Small micro-tears build up, the heel pad becomes irritable, and even simple tasks—like standing barefoot on hard floors—can feel uncomfortable.
For runners, this can be particularly disruptive. Each workout places thousands of impacts through the feet, and if footwear, surfaces, or mechanics aren’t ideal, stress concentrates at the heel and arch. Many runners notice the same cycle: pain with the first steps in the morning, easing after a warm-up, then flaring again later in the day or after a run.
What’s happening under the surface
The plantar fascia works like an energy strap under the foot. As your foot lands, it helps control pronation; as you push off, it stiffens the arch to make push-off efficient. It shares the workload with your calf, Achilles tendon, and small foot muscles.
When calves are tight or ankles lack mobility, the fascia absorbs more load. When arch muscles are weak, the fascia takes over even more of the work. Over time, the tissue fatigues and becomes painful. This explains why strengthening and stretching both play such a critical role in recovery.
Symptoms runners notice first
Sharp heel pain with the first steps in the morning or after rest
Tenderness at the inside of the heel and aching along the arch
Pain that eases as you move, then returns after a run or long day on your feet
Tight calves and limited ankle motion
Gait changes, such as limping or avoiding heel strike
These symptoms help distinguish plantar fasciitis from bone injuries like stress fractures.
How plantar fasciitis is diagnosed
Diagnosis is usually made clinically. A clinician will ask about recent training changes, footwear, and surfaces. They will press around the heel and arch to locate tenderness, check ankle flexibility, and observe your gait for excessive pronation or shortened stride. Imaging is rarely needed unless pain is severe, unusual, or not improving. The focus is not only to confirm plantar fasciitis but also to uncover the training errors or movement restrictions that triggered it.
Many people choose Physiotherapy at this stage to get a clear diagnosis and a tailored plan. A physiotherapist can also identify weaknesses or imbalances that put extra stress on the fascia.
The runner’s recovery framework
There isn’t a single fix. Lasting recovery requires a blend of reduced load, mobility work, strengthening, good footwear, and a gradual return to running.
Phase 1 — Calm the pain
The aim is to reduce irritation without losing fitness. Cut back or pause running and choose low-impact cardio like cycling, rowing, or swimming. Ice your heel for 10–15 minutes after activity. Taping or a night splint may ease pain by reducing strain overnight. Gentle calf pumps and ankle circles are safe starting points.
Massage Therapy can also help in this early phase by easing tight calf muscles and improving circulation in the foot. Even light hands-on work around the fascia can make walking more comfortable.
Phase 2 — Restore movement and strength
Once pain is manageable, introduce regular stretching and strengthening. Stretch the plantar fascia by pulling your big toe toward your shin for 30–45 seconds. Stretch both gastrocnemius (straight knee) and soleus (bent knee) for 30 seconds each side. Add strengthening with towel curls, short-foot holds, and heel raises. Begin seated, then progress to standing and eventually single-leg heel raises.
This is the phase where Physiotherapy exercise programs shine. Targeted drills not only strengthen the foot but also improve ankle and hip mechanics to keep the problem from coming back.
Phase 3 — Build resilience and reintroduce impact
When walking is pain-free and you can perform 20 single-leg heel raises without soreness, it’s time to prepare for running. Add slow, heavy calf raises, single-leg balance drills, and small hops. Once tolerated, start a graded walk–jog plan.
For stubborn cases, Shockwave Therapy may be added. It stimulates blood flow and speeds tendon and fascia healing, making it especially useful if progress has stalled with exercise alone.
A simple daily routine
Morning: ankle pumps and circles before standing, then 2–3 plantar fascia stretches
Midday: wall calf stretches (straight- and bent-knee) for 30 seconds each side
Evening: towel curls (2×15 reps) and heel raises (3×10 slow reps, progress to single-leg)
All day: supportive shoes indoors and outdoors to avoid extra stress on the fascia
If pain increases, scale back and apply ice for 10 minutes. Use the “24-hour rule”: mild soreness that eases the next day is fine; sharp or lingering pain means you’ve done too much.
Quick relief strategies
Roll the arch on a frozen water bottle for 5 minutes
Do calf pumps after sitting for long periods
Practice short-foot holds while brushing your teeth
Wear supportive slippers indoors during flare-ups
Simple recovery table
| Phase | Goal | Key Actions |
|---|---|---|
| 1. Settle | Calm pain & protect fascia | Rest or cross-train, ice 10–15 min, taping/night splint, calf pumps, seated heel raises, consider Massage Therapy |
| 2. Restore | Improve mobility & add strength | Plantar fascia & calf stretches, towel curls, short-foot holds, heel raises (seated → standing → single-leg), guided Physiotherapy |
| 3. Rebuild | Prep for running | Heavy calf raises, single-leg balance, gentle hops, walk–jog plan; add Shockwave Therapy if progress stalls |
Footwear and support
Shoes play a major role in both recovery and prevention. Retire worn-out trainers after 300–500 miles, sooner if you run mostly on hard surfaces. Runners with flat feet may benefit from stability shoes; those with high arches may need more cushioning. Arch supports or custom orthotics can reduce strain. Everyday shoes matter too—supportive footwear indoors and at work prevents setbacks.
If pain is affecting more than just your running, broader care for Ankle & Foot Pain is recommended. This includes evaluating gait, checking muscle imbalances, and ensuring that both running and daily footwear support your recovery.
Return-to-running plan
Start when you can walk briskly for 30 minutes pain-free and perform 20 single-leg heel raises without next-day soreness.
Weeks 1–2: alternate 1 minute jog / 2 minutes walk × 8–10. Progress to 90 seconds jog / 90 seconds walk × 8 if tolerated.
Weeks 3–4: transition to 20–30 minutes continuous easy running every other day. Add ~10% time each week if pain-free.
Week 5+: add a longer easy run and relaxed 20-second pickups. Add hills and speed last.
If pain returns, step back one phase and give tissues time to settle before progressing.
Long-term prevention
Increase mileage or intensity by no more than 10% per week
Vary running surfaces and avoid repeated hard or cambered ground
Keep strength and stretching routines year-round
Replace shoes on schedule
Get enough sleep, hydrate, and maintain a healthy body weight
Early warning signs to act on
Morning heel pain appearing suddenly
Arch tenderness after a new shoe or surface change
Calf tightness that doesn’t improve with warm-up
Subtle limp or shortened stride during easy runs
Respond early with lighter training, extra stretching, and supportive footwear. Addressing small niggles quickly prevents long lay-offs.
FAQs
Is this the same as a heel spur?
Not necessarily. Heel spurs are bony growths that often show up on imaging but aren’t always the source of pain. Plantar fasciitis is primarily a soft-tissue problem. Many people with spurs have no pain, and many with pain have no spurs.
Should I stop running completely?
Not always. During flares, reduce or pause running based on symptoms and keep cardio with low-impact options. Resume running only when walking is pain-free and strength markers are met. The plan above helps you progress safely.
Do I need orthotics?
Not everyone. Try supportive shoes first. Insoles can help if you overpronate, have flat or high arches, or if pain persists despite a solid program. Custom devices are most useful when foot mechanics are a key driver.
How long until I’m pain-free?
Mild cases may settle in a few weeks with consistent care. Chronic cases can take several months. The fastest recoveries pair graded loading with footwear fixes and smart training progression.
Can I stretch too much?
Yes. Aggressive, long holds on an irritable fascia can backfire. Keep stretches gentle and frequent, not forceful. Use the 24-hour response to guide dosage.



